- Home
- About
- Our Specialists & Specialties
- Cardiology
- Cardiovascular and Thoracic Surgery
- Dental Surgery
- Dr Aidan Yeo
- Dr Berenice Chan
- Dr Christopher Quek
- Dr Daylene Leong
- Dr Dennis Leong
- Dr Geraldine Oh
- Dr Henry Ho
- Dr Lam Ying Keat
- Dr Law Lay Yin
- Dr Leroy McCully
- Dr Poh Yu-Jin
- Dr Simon Ng
- Dr. Ang Chee Wan
- Dr. Boey Pui Yunn
- Dr. Bruce Lee
- Dr. Charmaine Tan
- Dr. Chong Yea Hwe
- Dr. David Tay
- Dr. Natalie Phoon
- Dr. Suraj Singh
- Dr. Wong Keng Mun
- Dermatology
- Ear, Nose and Throat Surgery
- Endocrinology
- Gastroenterology
- General Surgery
- Hand Surgery
- Infectious Disease
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics & Gynaecology
- Oncology
- Ophthalmology
- Orthopaedic Surgery
- Paediatric Medicine
- Paediatric Surgery
- Plastic & Reconstructive Surgery
- Respiratory Medicine
- Urology
Pain in the Neck
Posted by: Dr James Tan Siah Heng
Introduction
The neck (or cervical spine) performs a very important function of supporting the head and allowing full motion of the neck yet it must also protect the delicate spinal cord
Know your neck
Your neck bone consists of seven individual vertebrae with a soft cushion (disc) between each of them. Every time your nod or shake your head, these vertebral and disc work together to allow the neck movement and at the same time, protects the spinal cord. Muscles of your back of the skull, upper back and your shoulders are attached to these neck bones.
Causes of Neck Pain
There are many structures in the neck that can result in neck ache and pain. These are the common causes:
- Wear and tear (Spondylosis) – this refers to the wearing out (degeneration) of the intervertebral disc that acts as cushions between the individual neck bones. When the disc wears out, it can no longer support the neck as well as it used to be. The body tries to repair this by forming extra bone to act as supports and these are known as bone spurs (osteophytes). It is these osteophytes that cause compression on the nerves and spinal cord that result in some of the more severe symptoms.
- Disc herniation – when the disc wears out, it can also protrude outwards and this protruding disc that causes compression on the nerves that results in acute arm pain.
- Inflammation – this refers to the conditions like rheumatoid arthritis. This inflammatory process usually affects the fingers as well as other big joints like the knee joint. In the neck, it usually affects the upper cervical spine resulting in instability.
- Postural causes – this is the most common cause of neck pain. Prolonged postures of the neck in an unnatural position. For example, falling asleep on the sofa or prolonged working on the computer (especially on laptops) with the neck bent forward.
- Traumatic injuries – this can range from minor sprains to severe injuries as in whiplash injuries in car accidents.
- Other rare causes are infections, tumours and congenital abnormalities.
When is it serious?
Most of the time, the pain is self limiting – meaning that it will reduce over time with simple medications like paracetamol or NSAIDs with simple stretching exercises. It becomes serious when you have one or more of the following symptoms:
- Weakness – this means there is actual nerve compression and injury with damage to the nerve fibres. If left untreated, paralysis may occur.
- Numbnessor tingling– occasional numbness that goes away after a short period may be a sign of early nerve compression. If the numbness is persistent, it means nerve damage has already taken place and soon weakness will follow.
- Loss of bladder and bowel control – this is a very serious situation that warrants immediate admission to hospital and surgery. The presence of incontinence means severe spinal cord or roots compression that if left untreated, will result in permanent disability.
- Persistent pain on neck movement – the pain from neck sprains usual last from several days to one to two weeks. If the pain persists in severity and worsens over time, especially if it is associated with a fall or accident, there may be an undiagnosed neck fracture with instability.
- Pain that radiates down the arms – this radicular pain is caused by the nerve root being squeezed (usually due to herniated disc). Initially, it may just be pain but with time, tingling and weakness will develop.
What are the treatment options?
The main aim of the doctor would be to exclude serious conditions that can cause permanent damage. He will go through the history and performed an examination including a neurological examination to determine the state of the spinal cord and nerves.
The next step is imaging studies. There are several alternatives available:
- X-rays – This is simple and cheap but yields limited information. It is most useful to look for presence of instability.
- CT scans – This tool is good for looking at bony details but does not give sufficient information on the disc and spinal cord. Only option for those with metallic implants like pacemakers.
- MRI – Usually the investigation of choice as it provides a clear view of the state of nerve roots and spinal cord.
Treatment is always conservative first before resorting to surgery. Conservative options include:
- Rest (use of collar for a few days to reduce motion)
- Simple analgesia like paracetamol, NSAIDs.
- Exercises – stretching and strengthening
- Hot packs
- Modification of lifestyle
- Physiotherapy including traction.
Surgical options include:
- Fusion – a procedure where the damaged disc is removed and bone is inserted between the vertebras to fuse the level. This relieves the pressure on the nerve and spinal cord but it also increases the stress to the disc above and below the operated level.
- Arthroplasty (artificial disc replacement) – this is the newer approach where after disc removal, an artificial disc is inserted. This performs the same function as the disc by allowing motion at the operated level and reduces the damage to the adjacent discs.
- Laminectomy/ Laminoplasty – this is a time tested way to reduce pressure on the spinal cord over a large area by removing part of the bone. This surgery is performed from the back of the neck
- Facet Blocks – this is a minimally invasive technique to reduce neck pain, A fine needle is inserted from the side of the neck and local anaesthetic and steroid is injected to give relief to neck pain.
- Disc nucleoplasty – this is one of the latest minimally invasive methods to treat mild prolapsed disc and neck pain caused by disc degeneration. It involves using coblation technology to remove disc material.
Recent Articles
Lianhe Zaobao – 22th December 2011 Pancreatic Cancer and Bile duct Cancer are one of the rarest types of cancer. Pancreatic cancer is not a hereditary…
Read more- Our Specialities & Specialists
- CardiologyCardiovascular and Thoracic SurgeryDental Surgery
- Dr Aidan Yeo
- Dr Berenice Chan
- Dr Christopher Quek
- Dr Daylene Leong
- Dr Dennis Leong
- Dr Geraldine Oh
- Dr Henry Ho
- Dr Lam Ying Keat
- Dr Law Lay Yin
- Dr Leroy McCully
- Dr Poh Yu-Jin
- Dr Simon Ng
- Dr. Ang Chee Wan
- Dr. Boey Pui Yunn
- Dr. Bruce Lee
- Dr. Charmaine Tan
- Dr. Chong Yea Hwe
- Dr. David Tay
- Dr. Natalie Phoon
- Dr. Suraj Singh
- Dr. Wong Keng Mun
- CardiologyCardiovascular and Thoracic SurgeryDental Surgery
- Hand SurgeryInfectious DiseaseNephrologyNeurologyNeurosurgeryObstetrics & Gynaecology
- Dr Arthur Tseng
- Dr Brenda Low
- Dr Ching Kwok Choy
- Dr Choo Wan Ling
- Dr Cindy Pang
- Dr Jothi Kumar
- Dr Kelly Loi
- Dr Lee Keen Whye
- Dr Akhil Chopra
- Dr Leong Swan Swan
- Dr Tan Sing Huang
- Dr Tay Miah Hiang
- Dr Thomas Soh I Peng
- Dr Wong Nan Soon
- Hand SurgeryInfectious DiseaseNephrologyNeurologyNeurosurgeryObstetrics & Gynaecology
- Orthopaedic Surgery
- Dr Mathew Cheng Hern Wang
- Dr Chan Beng Kuen
- Dr Chong Keen Wai
- Dr Francis Wong Yoke Hae
- Dr Khong Kok Sun
- Dr Leslie Leong
- Dr Liang Te Shan
- Dr Ngian Kite Seng
- Dr Patrick Goh
- Dr Peter Lee Yew Chung
- Dr Tan Chong Tien
- Dr Tho Kam San
- Dr Wong Yue Shuen
- Dr Adeline Wong
- Dr Chan Kit Yee
- Dr Goh Han Meng
- Dr Ian Ong
- Dr Kenneth Chua
- Dr Lam Lee Hua Catherine
- Dr Liew Woei Kang
- Dr Nancy Tan
- Dr Phuah Huan Kee
- Dr Ratna Sridjaja
- Dr Tan Zhen Han
- Dr Tang Poh Lin Jenny
- Dr Wong Chin Khoon
- Dr Zainal Muttakin A.R.
- Orthopaedic Surgery
Copyright © 2026, Surgeons International Holdings Pte Ltd
(Registration No. 200308374R)
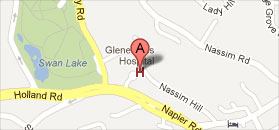
6 Napier Road, Suite 08-15, Gleneagles Medical Centre, Singapore 258499


 Locate us
Locate us Make An Appointment
Make An Appointment